DEFORMING OSTEOARTHRITIS
Deforming osteoarthritis is a chronic joint disease in which cartilage gradually deteriorates, bone structure changes, and deformities develop. 15 October 2025, Wednesday,
 33
33
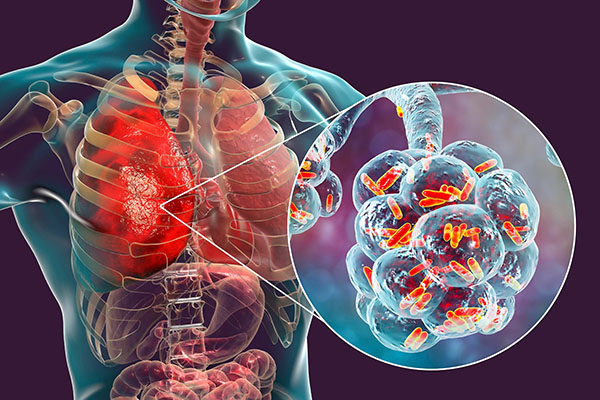
Community-acquired pneumonia is an acute infectious disease of the lower respiratory tract that develops outside the hospital setting or within the first 48 hours of hospital admission and affects the lung parenchyma.
Pneumonia is primarily caused by:
1․ Bacterial infections, which can be:
2․ Viral infections: Rhinovirus, Adenovirus, Influenza A and B, Coronavirus, and others
3․ In many cases, the causative pathogen is not identified.
Symptoms:
Fever, cough (productive or dry), dyspnea, chest pain, general weakness, tachypnea (>24 breaths/min), tachycardia (>100 bpm)
Auscultation findings in the lungs:
Decreased breath sounds, moist rales, crepitus, dullness to percussion.
Laboratory and instrumental investigations:
Adequate fluid intake, nutrition rich in protein and micronutrients
Moderate limitation of physical activity
Smoking cessation
Antipyretics and analgesics (e.g., acetaminophen or ibuprofen)
Empirical antibiotic therapy, chosen based on risk factors, comorbidities, individual characteristics (e.g., allergies), and clinical context
Antiviral therapy in case of viral etiology
